- Home
- About Dr. Nischay R
- Our Services
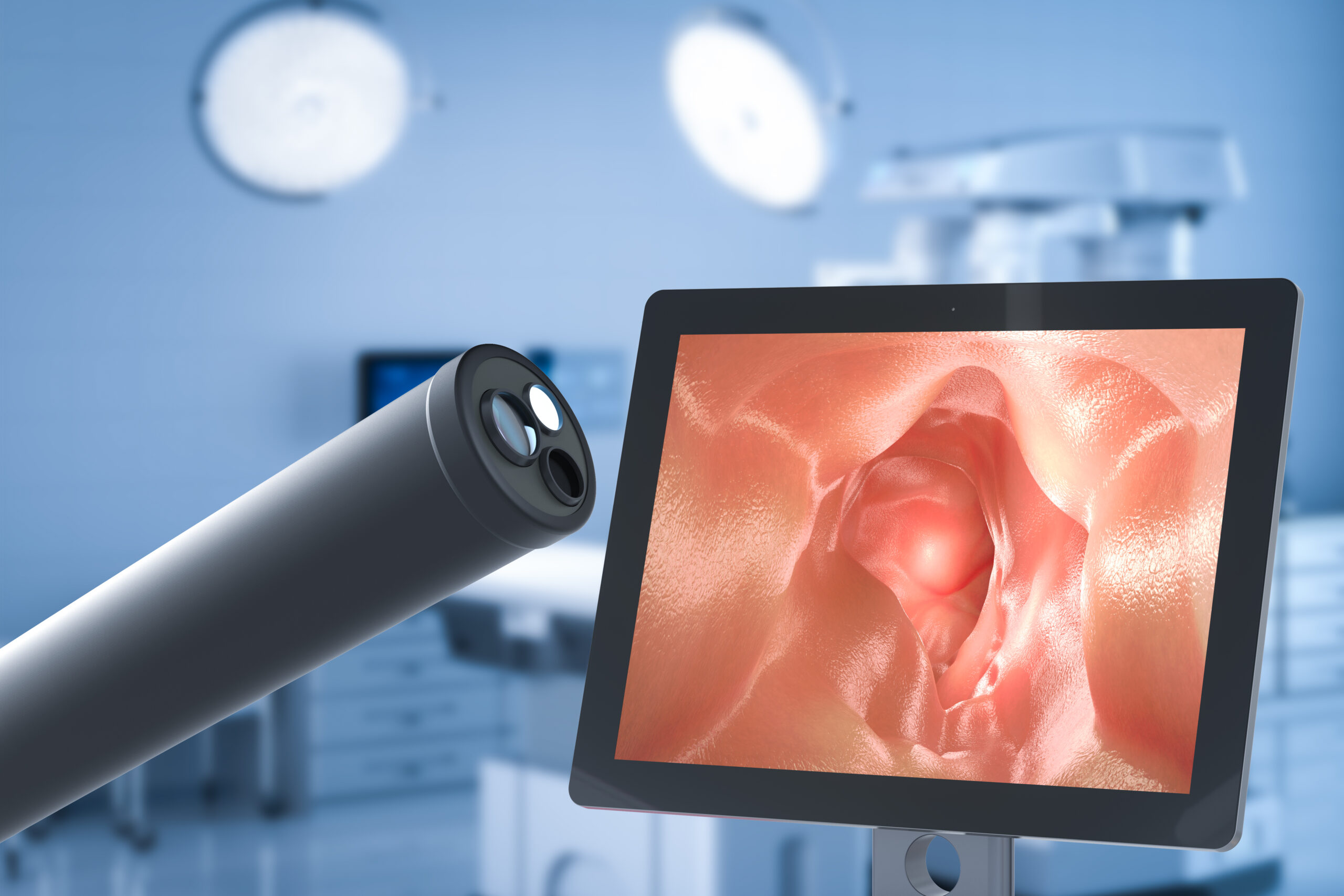
- Endoscopy
- Functional GI disorders
- Viral hepatitis
- Cirrhosis
- Colonoscopy
- Gastritis
- Autoimmune hepatitis
- Colitis
- ERCP
- Drug-induced liver injury
- Gastroenteritis
- Polypectomy
- Fibroscan
- GERD
- EUS
- Peptic ulcer disease
- Capsule Endoscopy
- Therapeutic Endoscopy
- Acute Pancreatitis
- Bile duct stones
- Chronic Pancreatitis
- Crohn’s disease
- Hepatobiliary tract malignancies
- Ulcerative colitis
Diagnostic Procedures
Diseases Treated
Gastrointestinal diseases
Hepatobiliary tract malignancies
Pancreatic Diseases
Inflammatory Bowel disease
- Contact Us